VENUE


DID YOU KNOW?
FACT 1*
FACT 2*
FACT 3*
FACT 4*
FACT 5*
FACT 6*
FACT 7*
FACT 8*
FACT 9*
FACT 10*

DISCOVER
EXCELLENCE

DR. MANISH SHAH
- Masters in Sleep Medicine
- General Medical Practitioner
- General, Implant and Cosmetic Dentist
- Certified in TMJ & Craniofacial Pain Management
After graduating from a degree in Dentistry with honours in 1998 (University of Sydney), Dr Manish went on to complete a degree in Medicine in 2005 (University of Sydney).
With a special interest in craniofacial pain and sleep disorders, Dr Manish has also competed a Masters in Medicine in Sleep Medicine (University of Sydney).
As a medical doctor and a dentist he has dedicated himself to providing wholistic care for all his patients.
Dr Manish has over 15 years experience in comprehensive restorative and cosmetic dentistry.

A/ PROFESSOR
narinder singh
Dr Narinder Singh is an ENT Specialist Surgeon, Clinical Associate Professor of Surgery at The University of Sydney (Australia’s oldest and largest medical school) and Chief of Otolaryngology, Head & Neck Surgery at Westmead Hospital, Sydney (Australia’s largest hospital campus).
Dr Singh is a Rhinologist, specialising exclusively in disorders of the nose and sinuses, including nasal obstruction, surgery for snoring/ OSA, complex and extended endoscopic sinus procedures, anterior skull base surgery and rhinoplasty (functional and aesthetic).
Dr Singh has a special interest in the role of nasal obstruction in the pathogenesis of dental and maxillo-facial disorders and is the “go-to” ENT surgeon for dentists, orthodontists and Maxillo-facial surgeons across Sydney and NSW.

Rochelle McPherson
Rochelle is one of Australia’s leading practitioners of Orofacial Myology. Her expertise are highly sought after in the industry, and she regularly conducts training and mentoring for other practitioners in this field both nationally and internationally.
Rochelle runs a private, orofacial myology practice in Sydney, OM Health, bringing a unique, holistic approach to patient care. She incorporates a team approach with other health professionals to assist in a greater level of health and well-being. Rochelle treats children of all ages through to adults. Her special interests include, Orofacial Growth and Development, Orofacial Pain and Sleep Disordered Breathing.
Rochelle is a lecturer at the Australian Academy of Orofacial Myology. She is committed to advancing Orofacial Myofunctional Therapy in Australia through best practice and continuing education.

Dr. Dimitrios Jim
Papadopoulos
Dr Papadopoulos is one of Australia’s leading sleep medicine physicians and is widely known for his work with sleep studies in children, and in particular children with AD/HD special needs, orthodontic problems, gastro-intestinal issues and need for CPAP therapy.
Dr Papadopoulos was admitted to FRACP in General Paediatrics in 2002.
In 2003 he became the first prospectively accredited Level 2 Paediatric sleep physician in Australasia (highest possible level).
He then established the Paediatric Sleep Unit at St George Private Hospital.
This continues to be the only Private Hospital Paediatric Sleep Unit in NSW to offer ASA/NATA accredited Paediatric Sleep Laboratory services including diagnostic studies and CPAP. Our first-in-Sydney ASA / NATA accreditation for these services, including a commendation for our CPAP service, makes us unique amongst paediatric sleep laboratories in Sydney.
ENQUIRE
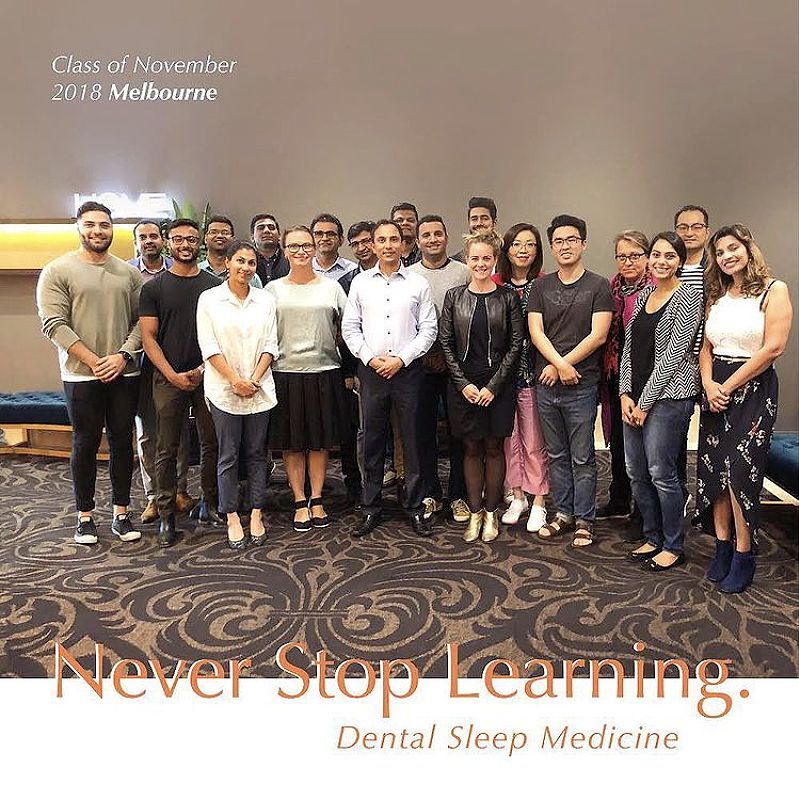
Testimonials
Speak Louder.
Join the Elites
Together, we achieve a higher vision.